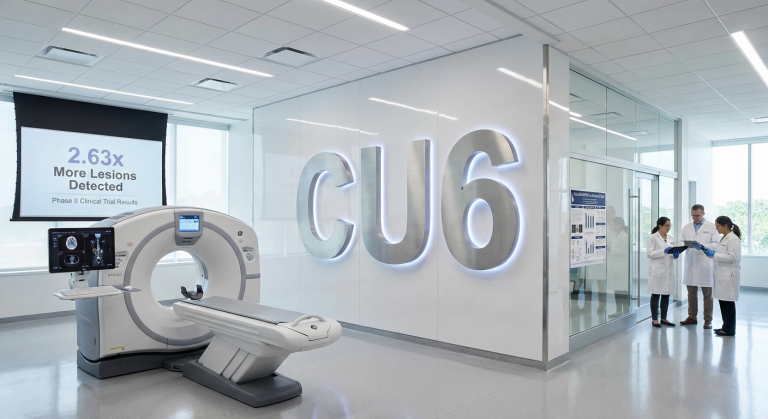
Clarity’s diagnostic outperforms standard-of-care by 2.6x in head-to-head prostate cancer trial
Clarity Pharmaceuticals (ASX: CU6) has released Clarity Pharmaceuticals Co-PSMA Trial Results demonstrating its 64Cu-SAR-bisPSMA diagnostic detected 2.63 times more lesions per patient than the current standard-of-care 68Ga-PSMA-11 in a Phase II head-to-head comparison. The mean per-patient lesion count was 1.26 for 64Cu-SAR-bisPSMA versus 0.48 for 68Ga-PSMA-11, with the difference achieving statistical significance (p <0.0001).
The Co-PSMA study was led by Prof Louise Emmett at St Vincent’s Hospital Sydney and enrolled 50 patients with biochemical recurrence of prostate cancer following radical prostatectomy. The abstract outlining key findings has been accepted for oral presentation at the European Association of Urology Congress 2026, Europe’s largest urological conference, scheduled for 13-16 March 2026 in London. The trial specifically targeted patients with prostate-specific antigen levels between 0.2-0.75 ng/mL, where current approved agents demonstrate limited detection capability.
This head-to-head data positions Clarity’s diagnostic product directly against the incumbent standard-of-care in a US PSMA imaging market valued at approximately US$2 billion annually, with projections to exceed US$3 billion by 2029. The results provide additional clinical evidence supporting the company’s registrational trial programme as it advances towards potential commercialisation.
What is PSMA PET imaging and why does detection sensitivity matter?
Prostate-specific membrane antigen is a protein expressed on prostate cancer cells. PET/CT imaging uses radioactive tracers that bind to PSMA to detect cancer lesions throughout the body. Current approved PSMA PET agents, including 68Ga-PSMA-11 and 18F-DCFPyL, are highly specific but demonstrate low sensitivity at low PSA levels, meaning they frequently fail to detect early-stage recurrence.
Biochemical recurrence occurs when PSA levels rise following initial treatment such as surgery or radiation, indicating cancer may have returned. Patients with early rising PSA often show no detectable disease on current standard-of-care scans, creating a clinical dilemma where clinicians know cancer is likely present but cannot locate it for targeted treatment. This detection gap makes treatment planning challenging and can result in delayed intervention.
The limitation of current diagnostics represents a significant unmet medical need in prostate cancer management. A diagnostic capable of detecting cancer earlier enables clinicians to intervene before disease spreads, potentially preventing progression to advanced stages. Earlier detection allows for targeted therapies such as salvage radiation to specific lesions, avoiding the side effects associated with systemic treatments like hormone therapy whilst the cancer remains localised and curable.
Trial results demonstrate step-change improvement in patient detection
The Clarity Pharmaceuticals Co-PSMA Trial Results showed 64Cu-SAR-bisPSMA next-day imaging detected prostate cancer in 78% (39/50) of trial participants, compared to 36% (18/50) identified by 68Ga-PSMA-11. The difference of 42 percentage points represents more than doubling the patient detection rate. Across all participants, 68Ga-PSMA-11 identified 24 lesions in total, whilst 64Cu-SAR-bisPSMA detected 63 lesions, equating to 2.6 times more lesions using Clarity’s product.
The true positive rate comparison further reinforces the diagnostic advantage. Among participants with an evaluable standard of truth, 64Cu-SAR-bisPSMA achieved a 75% (21/28) true positive rate versus 39% (11/28) for 68Ga-PSMA-11, nearly doubling the accuracy in correctly identifying cancer presence. Importantly, planned patient management changed in 44% (22/50) of participants following assessment of the 64Cu-SAR-bisPSMA scan, indicating the additional lesions detected had direct clinical relevance.
| Metric | 68Ga-PSMA-11 (SOC) | 64Cu-SAR-bisPSMA | Improvement |
|---|---|---|---|
| Patients with positive scan | 36% (18/50) | 78% (39/50) | +42 percentage points |
| Total lesions detected | 24 | 63 | 2.6x more |
| True positive rate | 39% (11/28) | 75% (21/28) | Nearly double |
The 44% treatment modification rate demonstrates real-world clinical utility. Detecting cancer in nearly four out of five patients versus only two out of five represents a fundamental improvement in diagnostic reliability for this patient population.
How the trial was designed
The Co-PSMA trial enrolled 50 patients with biochemical recurrence following radical prostatectomy, with PSA levels deliberately restricted to 0.2-0.75 ng/mL. This low PSA range specifically targets the patient population where current standard-of-care diagnostics demonstrate their poorest performance. All participants were candidates for curative salvage therapy and had received no prior salvage treatment.
Each participant underwent 68Ga-PSMA-11 PET/CT followed by 64Cu-SAR-bisPSMA PET/CT within three weeks, with both scans performed on the same digital PET camera to eliminate equipment variability. 64Cu-SAR-bisPSMA imaging was conducted at one hour and 24 hours post-injection, with next-day imaging used for the primary comparison. A standard of truth methodology determined scan accuracy through biopsy, response to targeted treatment without androgen deprivation therapy, or corroborative imaging.
The trial design specifically targeted the patient population where Clarity’s product differentiation is most pronounced. By restricting PSA to low levels, the study isolated the clinical scenario where improved detection sensitivity matters most for patient outcomes.
Results reinforce earlier COBRA trial findings
The Co-PSMA results align with data from Clarity’s completed COBRA trial, which also evaluated 64Cu-SAR-bisPSMA performance in patients with biochemical recurrence. COBRA enrolled patients with no upper PSA limit (median 0.9 ng/mL, range 0.25 to 17.6 ng/mL) and similarly demonstrated >2.6 times more lesions detected with 64Cu-SAR-bisPSMA compared to standard-of-care agents on next-day imaging (52.6 versus 20 lesions).
A subset of COBRA participants underwent follow-up standard-of-care PSMA PET scans at a median of 73.5 days after initial 64Cu-SAR-bisPSMA imaging. Despite the time interval allowing potential disease progression, 90% of these participants showed positive scans on initial 64Cu-SAR-bisPSMA next-day imaging, compared to only 60% positive on the later follow-up standard-of-care scan. This suggests 64Cu-SAR-bisPSMA detected lesions that remained undetectable on standard-of-care imaging even weeks later.
Dr Alan Taylor, Executive Chairperson
“What we are learning today from the head-to-head Co-PSMA study is a valuable insight into how 64Cu-SAR-bisPSMA directly compares against 68Ga-PSMA-11, further bolstering the data seen to date.”
Replication of the >2.6x lesion detection improvement across both Co-PSMA and COBRA trials, despite different patient selection criteria, strengthens the clinical evidence package. Consistent performance across independent studies reduces the likelihood results represent statistical anomaly or patient selection bias.
Commercial opportunity in US$2 billion PSMA imaging market
The current US market for PSMA PET imaging is valued at approximately US$2 billion annually, with growth projections exceeding US$3 billion by 2029. This market is presently dominated by 68Ga-PSMA-11 and 18F-DCFPyL, both approved agents with documented low sensitivity, particularly at low PSA levels. The substantial market size reflects widespread adoption of PSMA PET imaging as standard practice in prostate cancer diagnosis and recurrence monitoring.
Clarity’s 64Cu-SAR-bisPSMA has secured three FDA Fast Track Designations, signalling regulatory recognition of the unmet medical need and potential clinical benefit. The Fast Track programme is designed to facilitate development and expedite review of therapies treating serious conditions and addressing unmet medical needs. These designations provide the company with more frequent FDA interactions and eligibility for accelerated approval and priority review if relevant criteria are met.
The competitive landscape includes emerging products, but according to company commentary, the development pipeline offers no significant differentiation from existing agents. Some competitors are commercialising the unpatented 68Ga-PSMA-11 agent already capitalised on by three separate entities. This suggests limited innovation in the competitive field beyond Clarity’s dual-targeting bisPSMA approach.
Path to commercialisation
Clarity’s registrational trial programme comprises two studies nearing completion of recruitment:
- AMPLIFY registrational trial
- CLARIFY registrational trial
- EAU Congress 2026 oral presentation (mid-March 2026)
- Three FDA Fast Track Designations secured
The oral presentation of Clarity Pharmaceuticals Co-PSMA Trial Results at EAU Congress 2026 will include further data from the study. The conference represents Europe’s largest urological meeting and provides a platform for peer review by key opinion leaders in prostate cancer diagnosis and treatment. Acceptance as an oral presentation, rather than poster format, indicates the programme committee assessed the data as particularly significant.
The Co-PSMA study, whilst not itself a registrational trial, provides additional supporting evidence for the regulatory submission package. Head-to-head comparisons against standard-of-care strengthen the clinical value proposition by directly demonstrating superiority rather than relying on indirect comparisons across separate studies.
Why earlier detection changes patient management
Detecting cancer lesions earlier in the disease course enables targeted intervention before spread occurs. The 44% treatment plan modification rate in Co-PSMA demonstrates that additional lesions detected by 64Cu-SAR-bisPSMA had direct clinical impact on management decisions. Patients with newly identified lesions may become candidates for salvage radiation therapy targeting specific sites, rather than empirical systemic treatment.
Earlier intervention in biochemical recurrence can prevent cancer growth and metastatic spread. When lesions are identified whilst still localised, targeted therapies such as stereotactic body radiation therapy can eliminate disease with minimal side effects. Conversely, patients showing no detectable lesions on standard-of-care scans may be placed on active surveillance, potentially allowing micrometastatic disease to progress undetected.
Avoiding systemic therapies such as hormone ablation until absolutely necessary improves quality of life. Androgen deprivation therapy carries significant side effects including fatigue, hot flashes, reduced bone density, and metabolic changes. Targeted treatment of detected lesions can defer or eliminate the need for systemic therapy in patients with oligometastatic disease (limited number of metastases).
Prof Louise Emmett, Principal Investigator
“These findings highlight the potential for 64Cu-SAR-bisPSMA to improve patient outcomes.”
The clinical significance extends beyond immediate treatment decisions. Accurate staging enables appropriate patient selection for clinical trials, informs prognosis discussions, and establishes accurate baseline disease burden for monitoring treatment response. The 2.63-fold improvement in lesion detection translates directly into improved clinical decision-making across these multiple dimensions.
Get Healthcare News Before the Market Reacts
Join 20,000+ investors receiving FREE breaking ASX healthcare announcements within minutes of release, complete with in-depth analysis. Stay ahead on trial results, regulatory updates, and market-moving developments. Click the “Free Alerts” button at StockWire X to start receiving real-time alerts the moment news breaks.